Leukemia
Oncohematology Group
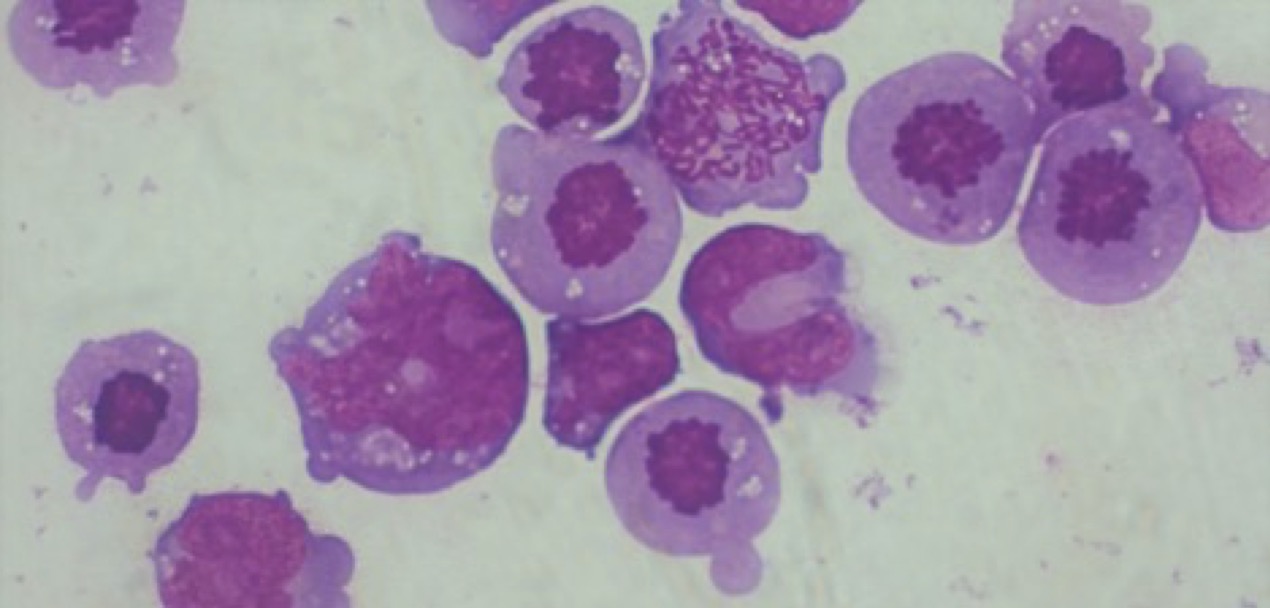
Acute Lymphoblastic Leukemia (ALL) and Acute Myeloid Leukemia (AML)
In the adult population, acute lymphoblastic leukemia (ALL) is a blood cancer characterized by the accumulation of immature lymphoid B-T cell progenitors. Conventional treatments for adult patients with ALL use a combination of vincristine, dexamethasone, cyclophosphamide or anthracyclines (chemotherapy regimen called Hyper-CVAD) that induces complete remission (CR) in 80-90% of patients. Despite initial success, 5-year survival rates remain in the 40% range as a large percentage of patients relapse or become resistant to such therapies. Similarly, acute myeloid leukemia (AML), is a blood neoplasm affecting immature precursors of the myeloid lineage (myeloblasts). This neoplasm has a higher incidence in adult individuals and in the elderly population. Like ALL, this leukemia must also be treated promptly with conventional chemotherapy regimens. In general, the five-year survival rate for adults with AML is about 25-30% with a relapse rate that depends on the type of AML.
Currently, the biological mechanisms underlying the progressive loss of efficacy of conventional treatments and the subsequent development of relapse are not fully understood. In recent years, numerous studies have shown that various factors such as tumor heterogeneity, tumor microenvironment, drug uptake/elimination and metabolism, regulation of apoptotic pathways, and DNA damage repair mechanisms (referred to as DNA Damage Response pathway, DDR pathway) can profoundly alter the efficacy of chemotherapeutic drugs. In particular, increased expression of DDR pathways has been shown to be associated with the onset of chemoresistance and poor prognosis in several tumor subtypes. The molecular mechanisms underlying the increased expression of genes involved of DNA repair mechanisms and their involvement in tumor development remain to be elucidated. In recent years, several innovative drugs have been developed that can selectively target several proteins involved in DDR pathways for the purpose of enhancing the effects of current chemotherapy therapies. Clinical and preclinical results have demonstrated the efficacy of these drugs however, it has not yet been defined which subtype of patients may benefit most from the use of these therapies. Our research activities are focused on the study of DNA damage response mechanisms in acute leukemias and the study of the biological and molecular mechanisms underlying the onset of chemoresistance.
Active projects 2023:
-FPS Grant “Understanding the role of DNA damage response in the development of chemoresistance and evaluating novel therapeutic strategies to overcome it”
PI: Andrea Ghelli Luserna di Rorà
FPS staff: Andrea Marranci, Francesco Olimpico
External collaborators: Prof. G. Martinelli (IRCCS-IRST), G. Simonetti (IRCCS-IRST), MT. Bochicchio (IRCCS-IRST), I. Iacobucci (St.Jude Childern Hospital,Menphis, USA), Prof. S. Galimberti (Hematology Unit, AOUP Pisa)
-Enhancing cpx-531 efficacy in secondary/therapy-related aml cells through the inhibition of DNA damage response pathway
Co-PI: Andrea Ghelli Luserna di Rorà
FPS staff: Andrea Marranci
External collaborators: G. Martinelli (IRCCS-IRST), G. Simonetti (IRCCS-IRST); G. Marconi (IRCCS-IRST)
-Synthetic Lethality for Personalized Therapy-based Stratification In Acute Leukemia (SYNtherapy)-ERA-Per-Med project
FPS staff: Andrea Ghelli Luserna di Rorà, Andrea Marranci
External collaborators: Prof. G. Martinelli (IRCCS-IRST), J.M. Hernández Rivas (Instituto de Investigación Biomédica de Salamanca, IBSAL), Prof. L. Bullinger (Charité University Medicine Berlin), Prof. Irit Gat (Tel Aviv Sourasky Medical Center), Prof. G. Castellani (University of Bologna).
-A multi-omic approach for gene fusion detection in hematological malignancies: towards improved diagnostic screening and therapeutic targeting – FUSION-TARGET
FPS staff: Andrea Ghelli Luserna di Rorà, Andrea Marranci
External collaborators: G. Martinelli (IRCCS-IRST), G. Simonetti (IRCCS-IRST); A.Ferrari (IRCCS-IRST); – C. Selleri (Azienda Ospedaliera Universitaria “San Giovanni di Dio e Ruggi d’Aragona”); G. Volpe (IRCCS Istituto Tumori Bari Giovanni Paolo II); E. Scarpi (IRCCS-IRST); AG. Solimando (Azienda Ospedaliero-Universitaria Consorziale Policlinico di Bari)